降血壓藥到底要不要吃?最新指導出爐原來又是財團壟斷
朋友寄來一則文章,沒有載明來源,搜尋之下,是日本良心名醫的一本書,朋友寄來文字中最讓我震撼的是這段:
高血壓標準值降低後,賺錢的是誰?
這個結果讓藥品產業笑得樂開懷。1988年日本國內的降血壓藥銷售額大約2千億日圓,到了2008年突破一兆日圓。藉著標準值的操作,藥品的銷售額暴增6倍。這種血壓藥的行銷手法可說非常成功。而且,標準制訂委員大多收取了製藥業者提供的鉅額獻金也是個問題。例如,包括高血壓標準在內的2005年日本版代謝症候群診斷標準制訂委員會成員中,11名國公立大學的醫師在2002至2004年的3年間,合計收取了高血壓等藥品廠商14億日圓的獻金。一直以來被視為有害物質的膽固醇,其實是「長壽之源」。1980年代,以長達5年時間追蹤福井市大約37000人的調查,獲得了明確的結果,亦即不論男女,膽固醇值最低的群組總死亡率最高,男性血液中膽固醇的值越高,總死亡率越低。但是治療的標準值並沒有因此而改變。降膽固醇藥也成為製藥業者的「搖錢樹」,生出以億,甚至以兆為單位的鉅額金錢。 希望大家不要理會檢查的數值,而要相信自己的體力。
除了日本的書外,還有最近的一則新聞提到美國政府2014年的指導方針,將60歲以上高齡人口高血壓標準從140/90(毫米汞柱)升高為150/90。之前到台大老人醫學科尋求醫生的意見,醫生建議減藥,回到原來心臟科醫生處,經過評估減一半,吃兩週後全部停藥,他建議160以上才吃藥。結果血壓又升高,但是不到160,按照心臟科大夫認為要160以上才吃藥,但是另外神經內科的醫生說要給藥,最後輪值親人認為要吃藥,讓吃降血壓藥回到原點。我想要不吃西藥改吃中藥,不知是否可行?如果是我自己就這樣作,但是老媽是大家的,可以這樣做嗎?請問觀世音菩薩還是基督耶穌呢?
搜尋到美國紐約時報的消息附在文末值得參考:
1. New guidelines published for managing high blood pressure
POSTED DECEMBER 18, 2013, 4:54 PM
Howard LeWine, M.D., Chief Medical Editor
Internet Publishing, Harvard Health Publications
2. 3 Things to Know About the New Blood Pressure Guidelines
By HARLAN M. KRUMHOLZ, M.D. DECEMBER 18, 2013,
3. Your blood pressure might not be as high as you think: Doctors say some older people may NOT need medication
@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@
美升高血壓標準 用藥人口少1/4
2014年3月30日 上午 06:32 GMT
(法新社華盛頓29日電) 研究今天顯示,如果按照美國最近發布的新指導方針,現階段接受高血壓治療的60歲以上美國民眾中,將有1/4不需再服藥。
杜克大學(Duke University)學者在「美國醫學會期刊」(Journal of the American Medical Association)表示,這代表美國有近600萬人未來不再需要以藥物控制血壓。
美國政府2014年的指導方針,將60歲以上高齡人口高血壓標準從140/90(毫米汞柱)升高為150/90。這項更動在醫界引發爭議,杜克大學的研究首次分析它帶來的衝擊。
美國國家高血壓預防、檢測、評估與治療聯合委員會(Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure)發布這項指導方針。
杜克學者分析2005-2010年美國全國健康營養研究調查(National Health and Nutrition Examination Survey)1萬6000名民眾資料,發現更改高血壓標準後,符合高血壓治療資格的美國成年人比例將從40.6%減少為31.7%。
此外,有1350萬成人不再處於高血壓危險區,其中580萬人將不再需要吃藥控制血壓。(譯者:中央社樂羽嘉) -----------
@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@
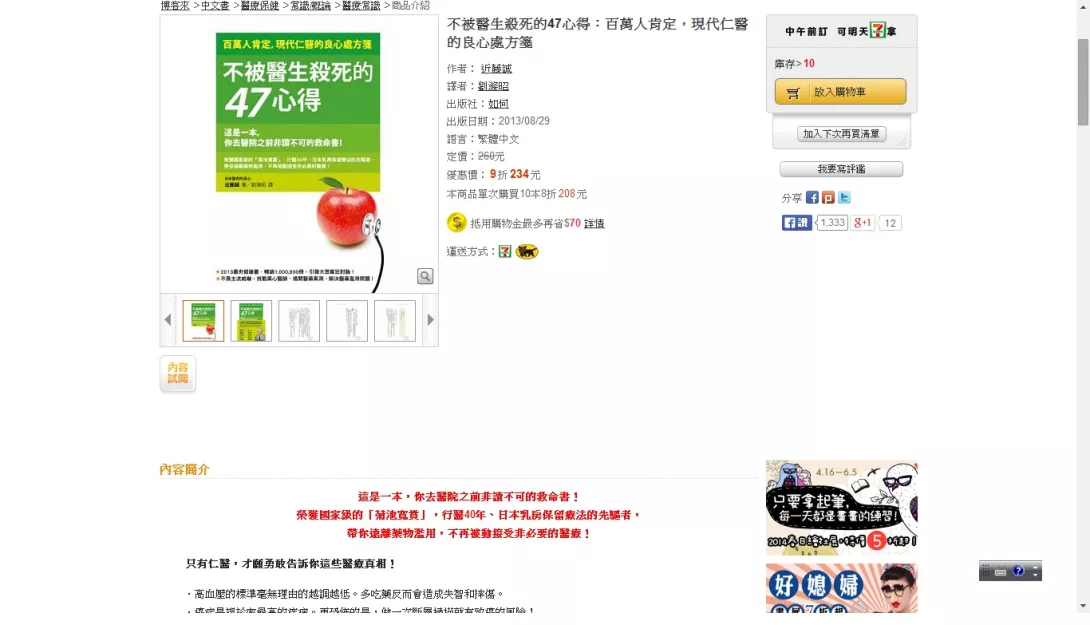
不被醫生殺死的47心得:百萬人肯定,現代仁醫的良心處方箋
作者:近藤誠
出版日期:2013/08/29
http://www.books.com.tw/products/0010596562
心得4「血壓一三○,生病了!」沒這回事
不能只看數值就以為生病
日本高血壓患者有四千萬人,高血脂患者有三千萬人……
「病人」的數目相當可觀。
高血壓和高血脂都有所謂的「標準值」。超過此數值就會被診斷為疾病。
例如,血壓的標準值,最高血壓(收縮壓)為一四○mmHg,最低血壓(舒張壓)為九○mmHg。超過此數值就是高血壓。
這個標準值很亂來,完全靠不住。
每一種疾病的標準值都由它的專門學會制定,但是這些數值都是經過協商,在沒有根據下做出決定的。特別是高血壓的標準值,「操作」的痕跡非常明顯。
一九九八年,厚生省全國調查時的標準值為一六○╱九五以上。
但是到了二○○○年,在沒有明確理由的狀況下降為一四○╱九○。依照一九九八年的標準值,日本的高血壓患者約有一千六百萬人,但根據新標準,患者人數即增加到三千七百萬人。
二○○八年開始的代謝症候群健康檢查,十九至六十四歲的人,若合併患有糖尿病或腎臟病,則血壓在一三○╱八○以上就被列為治療對象。
高血壓有九成以上原因不明。而且,日本也沒有關於降低血壓可使死亡率下降,或減少心臟病、腦中風發生率的實證資料。
成年之後,動脈會逐漸老化、變硬,將血液送出的力量相對減弱。
因此,為了將血液不斷送至腦部和手腳的每個部位,血壓會隨著年齡的增加而上升。如果使用藥物讓血壓下降,就可能造成失智或腳步蹣跚。
芬蘭曾經觀察五百二十一名「未服用降血壓劑」的七十五至八十五歲男女高齡者,結果發現八十歲以上,而且最高血壓超過一八○的人生存率最高,不到一四○的人,其生存率則明顯下降。
但是日本卻認為最高血壓超過一三○就是異常,而要求以藥物來降低。
@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@
心得44規畫持續工作到百歲的人生
工作至百歲成為常態的時代
二○一二年九月,一位「百歲的上班族」接受媒體訪問時說:「我從七十歲起任職至今的公司,是我人生中工作最久的地方。」並且表示,現在每天仍轉乘電車通勤。
同月,日本厚生勞動省發表,百歲以上的國民已超過五萬人。並推算到二○五二年時,達到百歲以上的人將突破七十萬人。
也就是說,現在六十歲以上的日本人中,有七十萬人四十年後仍然活在世上……
不久的將來,「百歲的上班族」不會再引起媒體注目,因為,一般人持續工作到八十歲、九十歲、一百歲的時代不久即將到來。
二○一三年四月,「老年人就業穩定新法」正式實施,退休年齡可延至六十五歲,但另一方面,政府的國家戰略會議中卻有人大膽提出「四十歲退休制」。這項提案的意圖是,「未來為了讓大家工作到七十五歲以上,不妨以四十歲左右作為人生的一個區隔。」
如果到了六十多歲大家都靠年金悠閒度日,相信社會很難承受。而且每個人對於自己成了社會包袱,時間還長達四十年之久,大概也會感到不安吧。
離死亡還很久
最近,摸索「死亡方式」成為大家關心的話題。「不希望失智或臥床拖累家人」「不想因治療而受苦」「不希望被視為社會包袱」……為了避免晚年吃苦頭而思考如何死亡。
但是,在進入天國之前,還有數十年的「緩衝時間」。
《日經商業》雜誌二○一二年九月十日號的特集<從隱居到持續工作至百歲的時代來臨>中,刊載了退休後如何度過充實生活的心得。
•早日學習適合社會環境的技術
•自發性的進行健康管理,以期能夠長期而健康的工作
•思考如何將過去培養的「人脈資產」轉移給下一代
•上班族時代的地位和自尊有百害而無一利
摸索著走向人類史上空前超長壽時代的我們,必須大幅改變想法。
退休後不是被社會環境「淘汰」,而是「走在前頭」。
不是永遠健康的「存活」,而是注意健康管理,以「持續工作下去」。
過去所培養的人際關係,不是「加深舊交」,而是「活用以反饋社會」。
上班族時代的地位和自尊,不再「擁抱不放」,而是「遺忘」。
這篇特集中還介紹了大貿易公司的退休職員,為了提升所有中小企業的競爭力而成立的「經營支援NPO俱樂部」。會員大約有一百六十人,雖然平均年齡達七○.一歲,但對於大量請求協助的案件仍能全力因應。
我過了六十歲後,曾覺得「或許大限之日即將到來」,但是看到「二○五二年時,一百歲以上的國民有七十萬人」的數字後,我改變了想法,認為如果每天等待大限之日到來,人將會麻痺,因此開始摸索人生的新舞台。
------------------------------------------------------------------------------------------------
1. New guidelines published for managing high blood pressure
POSTED DECEMBER 18, 2013, 4:54 PM
Howard LeWine, M.D., Chief Medical Editor
Internet Publishing, Harvard Health Publications
When it comes to your “health numbers,” your two blood pressure values are important to know—and keep under control. New guidelines for managing high blood pressure in adults, released this morning in a report inJAMA, aim to help doctors know when to start treating high blood pressure and how best to do it.
Millions of Americans have high blood pressure, also known as hypertension. It is the most common risk factor for heart attack and stroke. High blood pressure can also lead to kidney failure, aneurysm (weakening or bulging of blood vessel walls), damaged blood vessels in the eyes, and vascular dementia (the second leading cause of memory loss and thinking problems). Unfortunately, barely half of Americans with high blood pressure have it under control.
First, some background information. Blood pressure is the force exerted on the arteries by a wave of blood propelled from the heart. It is given as two numbers, each measurement recorded in millimeters of mercury (mm Hg), like 122/78. Systolic pressure (the top number of a blood pressure reading) gauges the pressure in the arteries at systole (SIS-tuh-lee), the instant when the heart contracts and pushes a wave of blood along the arterial tree (think “s” for squeeze). Diastolic pressure (the bottom number of a blood pressure reading) is the pressure during diastole (die-AS-tuh-lee), the brief period of relaxation between beats.
What the new guidelines fail to specify is what is “normal” blood pressure and what is high blood pressure. I’m going to stick with the current standard definitions:
Normal (meaning healthy) blood pressure: a systolic pressure under 120 and a diastolic pressure under 80.
Hypertension, or high blood pressure: a systolic pressure of 140 or higher and/or a diastolic pressure of 90 or higher.
What’s new
In a nutshell, here is what the new guidelines recommend:
among adults age 60 and older with high blood pressure, aim for a target blood pressure under 150/90.
among adults age 30 to 59 with high blood pressure, aim for a target blood pressure under 140/90
among adults with diabetes or chronic kidney disease, aim for a target blood pressure under 140/90.
The expert panel that put together the guidelines also weighed in on how best to get to these targets. It recommended that everyone with high blood pressure, as well as those in the gray zone between normal and high blood pressure, adopt healthy lifestyle changes known to control blood pressure. These include losing weight if necessary, limiting salt intake, eating a diet rich in fruits, vegetables, and whole grains, and keeping physically active.
When drug therapy is needed, the guidelines recommend starting with slightly different medications depending on race. For nonblacks, including those with diabetes, it’s okay to start with an ACE inhibitor, angiotensin-receptor blocker, calcium-channel blocker, or thiazide-type diuretic. Among blacks, including those with diabetes, a calcium-channel block or thiazide-type diuretic is the best initial medication. Among individuals with declining kidney function, it’s best to start with a low dose of an ACE inhibitor or angiotensin-receptor blocker, since these types of medications help protect the kidneys from further damage.
Creating guidelines always challenges the experts
The previous set of blood pressure guidelines, published 10 years ago, were put together by a panel assembled by the National Heart, Lung, and Blood Institute (NHLBI), and carried the gravitas of a federal recommendation. The current panel was assembled by the NHLBI in 2008, but then was essentially cut loose when the institute announced it wasgetting out of the business of developing clinical practice guidelines.
The panel set out to base their guidelines only on data from randomized controlled trials , the gold standard of medical research. They openly acknowledged that this wasn’t possible, and instead had to base some of the recommendations on expert opinion. The recommendations are sure to draw criticism and create some controversy. To their credit, the panelists have said they would share all of the prepublication comments and communications between experts within and outside the panel.
I applaud the panelists for what they have accomplished. This was an incredibly difficult task.
Take-home messages
Although the new guidelines address an area of controversy—how low should blood pressure go—they don’t change the basics:
Know your blood pressure. Take advantage of any chance you have to get your blood pressure checked. For example, many pharmacies have blood pressure devices that you can use for free. Or consider using a home blood pressure monitor.
Consider high blood pressure to be a reading of 140/90 or greater. If you have high blood pressure, you need to act. This might mean just getting another couple readings in the next few weeks. If it is much above 140/90, call your doctor’s office to arrange an appointment soon.
Lifestyle changes are important. Since our lifestyles are often what lead to high blood pressure, changes can help control blood pressure. Key places to focus are getting more exercise, improving diet, losing weight if needed, not smoking, and reducing stress.
Tailor treatment to your needs. No matter what the guidelines say, your blood pressure treatment and goals should be tailored to you personally. For example, a very old and frail person is more likely to feel better and have less fall risk with fewer medications and a blood pressure higher than 150 or even 160.
<h3 inline;\"="" style="font-size: 18px; margin-bottom: 14px;">Related Information: Diagnosis: Coronary Artery Disease
@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@
2. HEART
3 Things to Know About the New Blood Pressure Guidelines
By HARLAN M. KRUMHOLZ, M.D.
DECEMBER 18, 2013,
The long-awaited new hypertension guidelines will change how we approach patients with high blood pressure. Here are three things you should know about them.
First, the guidelines raise the systolic blood pressure (the top number of the blood pressure reading) threshold for drug treatment from 140 to 150 for people 60 and older.
You may be familiar with the idea that hypertension should be treated when your blood pressure is higher than 140/90 mm Hg. Now, based on studies, the experts suggest starting drug therapy only when the reading is 150/90 or higher. In fact, the authors, some of the most prominent experts in the diagnosis and treatment of high blood pressure, said that the goal of drug treatment is to lower the blood pressure below 150/90.
This recommendation immediately puts many people who had drug treatment started because of mild elevations in systolic hypertension in an overtreatment category. Many people currently on drug treatment would not have been recommended for treatment under these new guidelines, including those who had high-normal values and were being treated for so-called pre-hypertension, a condition never officially sanctioned for treatment.
Second, there is insufficient medical evidence to support a systolic blood pressure threshold for the drug treatment of people younger than 60.
Let me repeat that. After all these years of studying people with high blood pressure, the panel concluded that there was insufficient evidence to support a recommendation for this large segment of the population.
Now that did not stop the authors from expressing an opinion that we ought to stay with the current threshold of a blood pressure lower than 140 for those younger than 60. They argued that there was no reason to change what we have been doing – even though it has been based on opinion and not evidence. My take here is that the evidence for this threshold is weaker than most people might believe – and decisions about treatment need to acknowledge this uncertainty and defer to the preferences of patients.
The authors of the guidelines similarly also stated that we lack evidence for the right target for patients with kidney disease and diabetes. Given the lack of evidence, the authors settled on a recommendation of a goal of less than 140/90 for patients for people with kidney disease and also those with diabetes. This is a change for many people because many doctors have been seeking a systolic blood pressure goal of less than 130, but the authors noted that such a recommendation is not supported by any clinical trial.
Meanwhile, they do indicate that the diastolic blood pressure (the bottom number) should be less than 90, and for people age 30 and older there is evidence to support that recommendation.
Third, the guidelines recognize that the modification of a risk factor – in this case hypertension, which is a risk factor for heart attacks and strokes and premature death – by drug therapy does not necessarily mean that you have reduced someone’s risk for these adverse health events.
What we discovered in studies was that treating mild elevations of blood pressure with drugs does not reliably improve patients’ health. Although there is no question that drug treatment of very high blood pressure levels is beneficial, we now have several studies that failed to reduce risk by lowering blood pressure from mildly elevated to lower levels. Several studies sought to reduce risk by lowering blood pressure from mildly elevated to lower levels – and the surprising finding was that there was no benefit.
What this means is that drugs have many effects, and their effect on a single risk factor does not capture all they are doing and cannot convey their net effect on someone’s health. We have so many examples of trying to change risk factors with drugs and doing no good – or even harm – even as we make a single risk factor look better.
The authors of the guideline were influenced by these studies and did not default to the idea that more treatment is better. They reflected on what we know from studies that tested specific treatment strategies, which led them to be more conservative in their recommendations than previous guidelines.
Additionally, there are other important aspects of these guidelines. While they focus on drug treatment, they do emphasize the importance of a healthy diet, weight control and regular exercise. They make separate recommendations for black and white patients. They steer people away from beta-blockers for the treatment of high blood pressure. They steer black patients away from ACE inhibitors or angiotensin receptor blockers. They steer all people toward thiazide-type diuretics and calcium channel blockers.
In summary, this is a large paradigm change. The authors state that they did not intend to redefine what constitutes high blood pressure, but in effect they have now set it at 150/90 for the purpose of drug treatment of the general population. They have illuminated the weakness of our current body of evidence and made sensible recommendations given what we know.
The new guidelines are a reason for people being treated for high blood pressure to start 2014 with a discussion with their doctor, particularly if they started drug treatment for mildly elevated blood pressure. As always, all decisions about your treatment should reflect your own preferences about whether the benefits are worth the risks. What these guidelines reveal is that many decisions about blood pressure treatment are being made with less evidence than we need. This is a call to action for studies that can equip patients facing decisions about treatment with the information they need.
Harlan Krumholz is a cardiologist and the Harold H. Hines Jr. Professor of Medicine, director of the Yale-New Haven Hospital Center for Outcomes Research and Evaluation and director of the Robert Wood Johnson Clinical Scholars Program at Yale University School of Medicine.

回應文章建議規則: